Gynecology
Urogynecology Clinic
Urogynecology is a medical specialty that deals with diseases located at the boundary between "urology" and "gynecology".
The Urogynecology Clinic is a specialized outpatient clinic for female-specific conditions such as pelvic organ prolapse (including uterine prolapse, cystocele, and rectocele) and urinary incontinence.
If you are experiencing any of the following symptoms, please do not hesitate to consult us rather than worrying alone:A feeling of something descending from the vaginal area causing discomfort,a sensation like a ping-pong ball coming out from the vagina, feeling as if something is caught in the pelvic area, difficulty urinating, frequent urination, urinary leakage or fecal incontinence.
Pelvic organ prolapse occurs when the supporting tissues of the pelvic organs become weakened. It affects approximately one in four women.
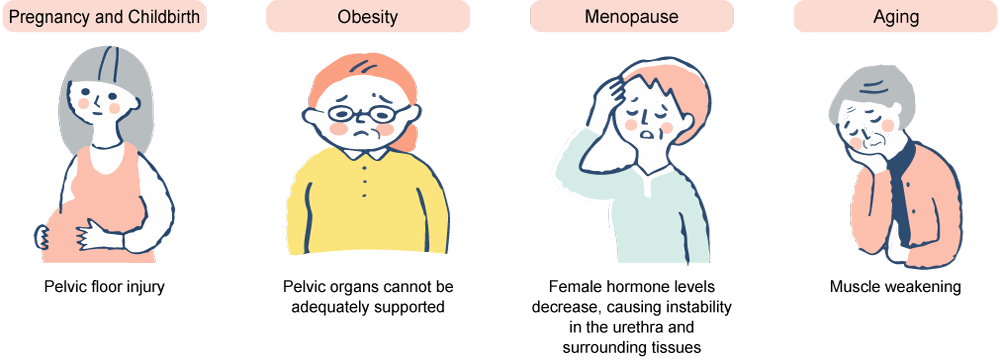
Possible causes include pelvic floor injury due to pregnancy and childbirth, inadequate support of pelvic organs due to obesity, decreased female hormone levels during menopause leading to instability of the urethra and surrounding tissues, and weakening of the muscles associated with aging.
Since the symptoms and causes vary for each individual, we strive to propose treatment options that are tailored to each patient’s specific needs.
While pelvic organ prolapse and urinary incontinence are not life-threatening conditions, they can significantly affect quality of life. Many patients who have undergone treatment for pelvic organ prolapse have reported feeling much more comfortable afterward. We hope that our treatments can help improve your comfort and vitality in daily life moving forward.
Examinations will be conducted by a female obstetrician-gynecologist.
If a detailed urological evaluation is necessary, we will refer you to our hospital’s urology department.
Target Conditions
Pelvic Organ Prolapse
Pelvic organ prolapse (cystocele, uterine prolapse, vaginal vault prolapse, enterocele, rectocele)
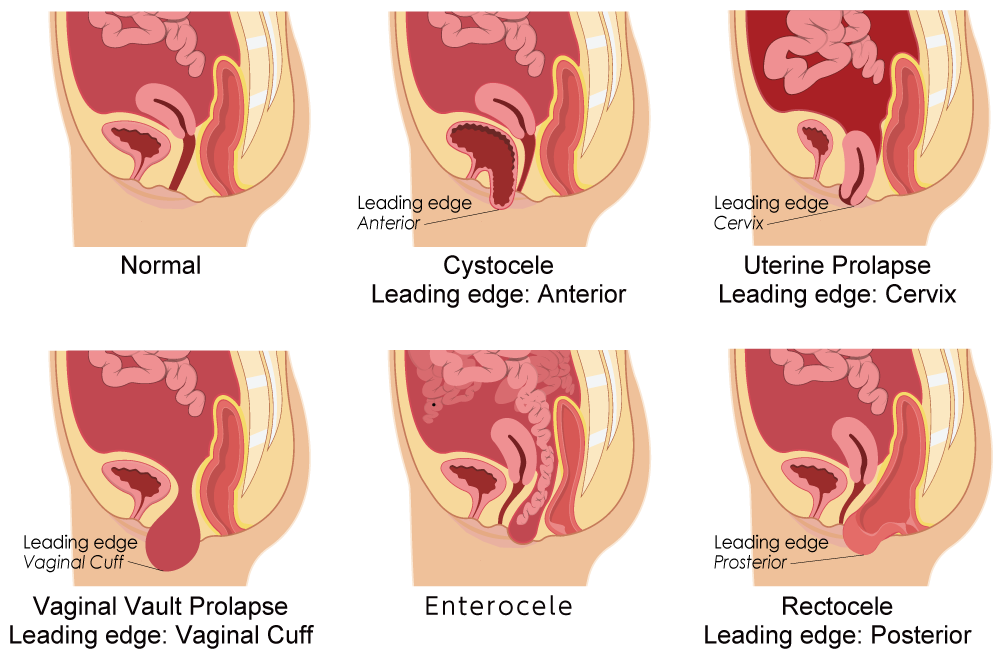
Pelvic organ prolapse refers to a condition in which the supporting tissues of the pelvic floor become weakened, allowing the pelvic organs (such as the bladder, uterus, small intestine, and rectum) to protrude through the vagina.
When the bladder descends through the vaginal wall, it is called a cystocele; when the uterus descends, it is called uterine prolapse; and when the small intestine or rectum descends, it is called an enterocele or rectocele, respectively.
In individuals who have previously undergone hysterectomy, the vaginal vault itself may invert and descend, a condition known as vaginal vault prolapse.
Types of Pelvic Organ Prolapse
Types of Urinary Incontinence
In collaboration with the urology department, we provide diagnosis and treatment for various types of urinary incontinence.
Treatment Options
Conservative therapy (such as pelvic floor muscle exercises and pessary therapy)

For patients with mild pelvic organ prolapse symptoms or those who do not wish to undergo surgery, we recommend outpatient guidance on pelvic floor muscle exercises or the use of a pessary (a vaginal support device).
Surgical Treatment
For patients with severe pelvic organ prolapse or those who wish to undergo surgery, we will discuss and provide surgical treatment tailored to the type and severity of the prolapse, the patient’s age, comorbidities, body type, and other individual factors.
| Surgery without mesh | Traditional vaginal hysterectomy, vaginal wall repair, and colpocleisis. |
|---|---|
| Surgery using mesh | TVM surgery (transvaginal mesh surgery), laparoscopic sacrocolpopexy, and robot-assisted sacrocolpopexy. |
In addition, pelvic organ prolapse is often associated with urinary incontinence, and for patients requiring surgical treatment for incontinence, we will also perform urinary incontinence surgery.
-
① TVM Surgery (Transvaginal Mesh Surgery)

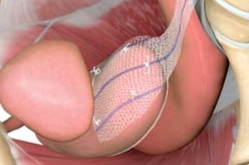
A mesh is inserted through the vagina and fixed to the pelvic ligaments to support and lift the prolapsed bladder like a hammock. This surgery is considered minimally invasive, allows for uterine preservation, and has a low recurrence rate.
-
② Laparoscopic Sacrocolpopexy (LSC)
Using a laparoscope, mesh is attached to the anterior and posterior vaginal walls and the vagina is lifted and fixed to the sacrum. As this is a laparoscopic procedure, postoperative pain from incisions is minimal, and there is less bleeding and a lower risk of mesh erosion. The vagina is restored to its natural state, preserving sexual function. This procedure is recommended for relatively younger patients who are sexually active.
-
③ Robot-assisted Sacrocolpopexy (RSC)
Sacrocolpopexy is performed with robotic assistance. This approach allows for more delicate maneuvers that are not possible with the camera used in standard laparoscopic surgery.
-
④ Vaginal Hysterectomy
The uterus is removed transvaginally. Portions of the prolapsed bladder and rectum are sutured, and the vaginal wall is narrowed by stitching.
This procedure is recommended for patients with comorbidities that increase the risk of infection and for whom mesh cannot be used. -
⑤ Colpocleisis
The vaginal mucosa is thinned and sutured together from the front and back to completely close the vaginal canal.
This surgery is recommended for older patients who are not sexually active. -
⑥ TVT/TOT Surgery for Stress Urinary Incontinence
This method involves securing the mid-urethra with a mesh tape. Placing the mesh tape under the urethra helps improve urinary incontinence symptoms.
The Urogynecology Clinic is open on Tuesday, Thursday, and Friday mornings.
Please feel free to consult with us.

